Dr. Garth Slysz, Guest Post: After Antibiotics
A clear, well researched, and compelling argument for not relying solely on probiotics to restore the gut microbiome after taking antibiotics. Rather, a fiber diet.
Garth Slysz is a friend, and was also the hospital physician who treated my mother in her last days. I have come to know him as a dedicated and caring physician, and one who is also interested in keeping up with the latest research in his field. He is also indirectly involved in some active research himself, carried out by his son Josh, who is a Prof. at Dalhousie.
He was motivated to write this piece by some important new groundbreaking research recently reported in Nature regarding the response to antibiotics in mice. The implications for health and diet discussed here are significant, so I thought it would be useful to reprint his piece (with his permission), here.
—LMK
What should we do?
MAY 06, 2025
Each prescription can raze your inner ecosystem. The way back isn't probiotic capsules but the careful art of ecological gut biome succession. A new study says feed them and they will come.
At 3 AM, the septic patient's fever finally broke after twelve hours of IV antibiotics. Our barometers show normalized blood pressure, reduced white counts, dropping CRP. But behind these numbers, in the unseen darkness of the gut, a massacre unfolds. Within 48 hours, this patient will lose upwards of a trillion microbes that serve as metabolic regulators, neurotransmitter factories, and hormone recyclers. They were converting fiber to fuel, neutralizing toxins, synthesizing vitamins. How long will it take for all this to come back online?
Two out of three North Americans will take antibiotics this year; half those prescriptions are unnecessary. Each course tilts internal ecosystems toward collapse, rewriting the metabolic code of our bodies in ways we're only beginning to understand.
As a physician, my understanding of what follows antibiotics has evolved dramatically. Not long ago, we barely considered the microbiome. "Eat some yogurt," we'd say casually. As awareness grew, prescribing probiotics became routine. Now we're learning that neither approach addresses the fundamental challenge.
Antibiotics can be like wildfires. Narrow-spectrum ones prune weeds; broad-spectrum varieties torch the canopy. A typical course drops bacterial diversity by 25-50%. Opportunists, like C. difficile, bloom in the aftermath. The gut becomes permeable. Low-grade inflammation persists.
But after every forest fire comes predictable succession of flora. First, pioneer species colonize bare ground. Then specialized young growth builds networks through root systems. Finally, mature canopy species return to form climax ecosystems. Our guts follow similar stages of regeneration.
The Lost Landscape
Our gut ecosystems were once naturally resilient. In the 1920s, rural Americans consumed 40-60 grams of fiber daily, enough complexity to weather occasional disturbances. The microbes in our great-grandparents' guts processed this wealth of plant material with deep redundancy built into every interaction.
Then came the Western diet. By the 1970s, fiber intake had plummeted to below 15 grams daily. We switched from complex carbohydrates to simple sugars, from whole grains to refined flour. Our microscopic ecosystems became dominated by a few species while specialists starved.
This degraded baseline meant antibiotics no longer disturbed resilient systems; they obliterated fragile ones. What our ancestors could have weathered became devastating for modern microbiomes.
The Science of Recovery
A groundbreaking 2025 study published in Nature crystallized this understanding. The research team, led by M. S. Kennedy at the University of Chicago, designed an experiment so simple yet revelatory that it will force a complete reconsideration of post-antibiotic recovery strategies.
They gave identical antibiotics (a triple antibiotic cocktail of vancomycin, neomycin, and cefoperazone, administered via drinking water for 72 hours) to two groups of mice. One group consumed a fiber-rich diet, mimicking the high plant-based intake of humans in the early 1900s. The control group ate standard chow approximating today's Western diet (low-fiber, high-fat).
The results defied expectations. Mice on fiber-rich diets began rebounding quickly, with biomass recovering to baseline levels by day 4 and phylogenetic diversity starting to recover after day 5, eventually reaching over 50% of baseline by day 11. Their microbiomes followed a rapid successional process, where early facultative anaerobes like Enterococcaceae and Lactobacillaceae dominated initially, followed by a gradual increase in stricter anaerobes over the first two weeks.
The Western diet mice? They remained in what the paper called "arrested succession," dominated by a single genus within Streptococcaceae (typically Lactococcus species) for up to four weeks.
Then came the experiment with significant implications for microbial therapies like probiotics and fecal transfer. Their researchers harvested microbiomes from healthy, diverse mice and transplanted them into the Western diet group. The transplants colonized briefly, then collapsed. Analysis revealed that beneficial anaerobes couldn’t establish in the intestinal environment starved of proper substrate, likely due to impaired biofilm formation caused by reduced butyrate and mucin production. The transplanted bacteria essentially bounced off the gut wall like rubber balls on concrete.
The Kennedy study challenges conventional approaches to microbial therapy, demonstrating that the host diet shapes the gut environment, determining which microbial species can thrive. In the absence of sufficient dietary substrates, transplanted microbes struggle to establish, behaving more like transient visitors than permanent residents.
The study illuminated the mechanisms behind this failure. In fiber-poor environments, a dominant taxon monopolized limited resources without releasing syntrophic byproducts, leading to a 73% reduction in butyrate production. This metabolic shift impaired mucin synthesis and gut barrier function, creating a cycle where reduced nutrient availability further hindered microbial establishment and epithelial health.
The findings also highlight challenges with microbial interventions like probiotics. The study showed that microbial transplants failed to promote recovery in fiber-poor conditions, suggesting that many commercial probiotic formulations, often prioritizing shelf stability and industrial processing over ecological compatibility, may face similar limitations. For instance, species like Lactobacillus acidophilus, a common probiotic, have shown limited effectiveness in other models when dietary substrates are lacking, consistent with the dietary dependency observed here. Meanwhile, species like Bacteroides thetaiotaomicron, which are critical for processing complex carbohydrates, require specific dietary fibers to survive and support a healthy ecosystem.
The researchers concluded, "Intervention experiments reveal that an appropriate dietary resource environment is both necessary and sufficient for rapid and robust gut microbiota recovery, whereas microbial transplant is neither."
The $90 Billion Misunderstanding
The probiotic market, projected to exceed $90 billion by 2027, rests on treating ecosystems as collections of individual species rather than as integrated networks. Marketing departments sell "diverse probiotic blends" with impressive species counts, but these formulations ignore syntrophic relationships, the sequential metabolic cooperation between microbes that make ecosystems function.
Consider Bifidobacterium adolescentis, marketed as a keystone probiotic for its purported benefits to infant gut health. In reality, B. adolescentis depends on complex oligosaccharides processed by other species first. Without Akkermansia muciniphila to break down mucin glycans, without Bacteroides species to pre-digest plant polysaccharides, B. adolescentis exists as an expensive tourist rather than an established resident.
The industry's focus on CFU counts (colony-forming units) reflects this ecological limitation. Ten billion CFUs of mismatched species create less functional recovery than ten million CFUs of properly networked microbes. It's the difference between dumping ten billion oak tree seeds onto bare ground versus carefully planting integrated forest communities that support each other's growth.
The supplement industry may benefit unintentionally from suboptimal outcomes. When patients consume probiotics without proper dietary foundation, the resulting incomplete recovery can drive continued purchasing. Such limitations point to a deeper philosophical error in how we approach microbiome recovery.
When Science Meets Reality
While the Kennedy study examined mouse models, its ecological principles align with decades of human microbiome research and clinical observation. These failures in probiotic-only approaches force us to confront a fundamental truth, that our microbiomes require substrates, not just supplements.
Certainly, antibiotics save lives. When sepsis threatens, when pneumonia advances unchecked, when C. difficile overwhelms a compromised system, they become necessary interventions. The goal isn't avoidance but understanding aftermath.
As physicians, we cannot await perfect replication studies while patients suffer needlessly from post-antibiotic sequelae that dietary intervention could address. Translation to human care requires wisdom over caution. A systematic, fiber-rich dietary protocol carries virtually no risk while offering profound potential benefits. Whether the three-stage recovery pattern precisely mirrors mice or follows its own human timeline, the fundamental principle remains that microbiomes recover through substrate provision, not pharmaceutical shortcuts alone.
For the 90% of patients prescribed antibiotics for community infections including bronchitis, sinusitis, and routine UTIs, this systematic dietary approach transforms antibiotic aftermath from microbiome disaster to opportunity for renewal. We needn't wait for perfect human trials to apply the common sense our grandparents had. My mom and grandmother insisted that I make sure I ate some ‘roughage’.
Here's what we can recommend with confidence:
Three Stages of Return
Recovery follows predictable succession:
Stage 1: Pioneer Species (Days 1-7)
Facultative anaerobes colonize first so start with beans, carrots, lentils and broccoli. These are hardy species that handle oxygen-rich conditions post-antibiotics. Bifidobacterium longum and B. adolescentis express α-galactosidases that crack raffinose oligosaccharides, while Lactobacillus species metabolize cellobiose. These pioneers release crucial metabolites:
acetate – sets acetate ratios needed by butyrate producers
malate – feeds Eubacterium hallii for butyrogenesis
citrate – fuels Roseburia species
Key substrates: Raffinose (beans, lentils, chickpeas, soybeans), cellobiose (lightly steamed broccoli and cauliflower), arabinan (carrot peel, sugar beet pulp). Target dosing: 3-5g raffinose, 2g cellobiose, 3g arabinan daily. Introduce with polyphenol-rich foods to accelerate anaerobic conditions.
Stage 2: Network Formation (Weeks 2-4)
Now that we have citrate, acetate and malate, we need resistant starches, onions and garlic. Specialized feeders establish syntrophic cross-feeding networks essential for diversity. R. bromii's amylosomes transform resistant starch to malto-oligosaccharides, which F. prausnitzii and Roseburia spp. convert to butyrate. Bacteroides coprocola and Prevotella copri break down arabinoxylan, producing acetate/lactate that E. rectale and Anaerostipes caccae transform into butyrate.
Key substrates: Resistant starch type 2/3 (green banana flour, retrograded rice/potato-cooling creates 2-7% resistant starch), partially hydrolyzed arabinoxylan (~2-5g), inulin-type fructans DP 10-25 (Jerusalem artichoke, onions, chickory, garlic). These fibers drive the metabolic networks that prevent microbial monopolies.
Stage 3: Climax Community (Months 2+)
Now we have the lacate and butyrate needed by the keystone species that maintain barrier integrity return. B. bifidum's surface β-galactosidases metabolize galacto-oligosaccharides to produce short-chain fatty acids that directly nourish goblet cells. Akkermansia muciniphila upregulates mucin turnover and tight-junction genes (claudin-1, occludin). These species maintain the mucus layer and epithelial barrier essential for long-term health.
Key substrates: GOS 5-8g daily (equivalent to ~150g peas), arabinogalactan (~1g), pectin-polyphenol complexes. These specialist fibers prevent enterobacteria overgrowth while supporting beneficial strict anaerobes. The 30-plant challenge provides substrate breadth that prevents functional loss during environmental perturbations.
Patients may experience brief discomfort as oxygen-sensitive anaerobes multiply. Temporary gas as fermenting fibers feed hungry pioneers. These are signs of regeneration, not failure.
What We Know and What We Don’t Know Yet
What We Know
A high-fiber diet is essential for microbiome recovery after antibiotics, outperforming microbial transplants in mouse models. The Kennedy study showed that mice on a fiber-rich diet recovered biomass by day 4 and over 50% of phylogenetic diversity by day 11, following a rapid successional process (Kennedy et al., 2025, Nature).
Diet shapes the gut environment, enabling syntrophic cross-feeding networks that support microbial diversity. In fiber-poor conditions, a dominant taxon monopolizes resources, reducing butyrate production by 73% and impairing gut barrier function (Kennedy et al., 2025).
Specific fibers support distinct recovery stages: raffinose and cellobiose feed pioneer species like Bifidobacterium and Lactobacillus, while inulin and resistant starch promote networking species like Faecalibacterium prausnitzii and Bacteroides coprocola (Pokusaeva et al., 2011; Ze et al., 2012).
Probiotics face ecological challenges, often failing to establish without proper dietary substrates. Many commercial formulations prioritize shelf stability over compatibility, limiting their effectiveness (Sanders et al., 2019, Nature Biotechnology).
Ecological succession principles apply to gut recovery, with predictable stages (pioneer, network formation, climax community) that can be supported by diverse plant-based foods, such as legumes, brassicas, and Jerusalem artichokes (Costello et al., 2012, Science).
What We Don’t Know Yet
How closely do the timelines of microbiome recovery in humans mirror those in mice, and do the same dietary interventions yield similar successional patterns?
What are the optimal fiber doses and types for individual humans, given variations in baseline microbiota, genetics, and health conditions?
Can we add SCFAs artificially to the diet to speed up microbiome recovery, and would this approach complement or disrupt natural microbial fermentation?
Can we develop probiotic formulations that better integrate with native microbial networks, and if so, what species and delivery methods would be most effective?
What long-term impacts does repeated antibiotic exposure have on microbiome resilience, and how can dietary strategies mitigate cumulative damage over time?
Conclusion
The path forward requires understanding of the ecosystems we harbor. While mice aren't humans, the principles of ecological succession remain universal. Each meal becomes an act of husbandry, feeding the trillions of allies that make us healthy. Feed them and they will grow.
Disclaimer: These dietary recommendations are general guidelines based on mouse studies and human nutrition research. Always consult with healthcare providers before making dietary changes, especially during recovery from surgery or with pre-existing conditions.
References
Costello, E. K., Stagaman, K., Dethlefsen, L., Bohannan, B. J. M., & Relman, D. A. (2012). The application of ecological theory toward an understanding of the human microbiome. Science, 336(6086), 1255-1262. https://doi.org/10.1126/science.1224203Kennedy, M. S., Freiburger, A., Cooper, M., St George, M. L., Kalski, M., Cham, C., Guzzetta, A., Ng, S. C., Chan, F. K., DeLeon, O., Rubin, D., Henry, C. S., Bergelson, J., & Chang, E. B. (2025). Diet outperforms microbial transplant to drive microbiome recovery in mice. Nature. https://doi.org/10.1038/s41586-025-08937-9
McDonald, D., Hyde, E., Debelius, J. W., Morton, J. T., Gonzalez, A., Ackermann, G., ... & Knight, R. (2018). American Gut: an open platform for citizen science microbiome research. mSystems, 3(3), e00031-18. https://doi.org/10.1128/mSystems.00031-18
McFeeters, R. F., Barrangou, R., & Klaenhammer, T. R. (1999). Cellobiose and other carbohydrates in fermented vegetables. Journal of Food Science, 64(5), 881-885. https://doi.org/10.1111/j.1365-2621.1999.tb15929.x
Pokusaeva, K., Fitzgerald, G. F., & van Sinderen, D. (2011). Carbohydrate metabolism in Bifidobacteria. FEMS Microbiology Reviews, 35(5), 897-914. https://doi.org/10.1111/j.1574-6976.2011.00272.x
Sanders, M. E., Merenstein, D. J., Reid, G., Gibson, G. R., & Rastall, R. A. (2019). Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nature Reviews Gastroenterology & Hepatology, 16(10), 605-616. https://doi.org/10.1038/s41575-019-0173-3
Slavin, J. (2013). Fiber and prebiotics: mechanisms and health benefits. Nutrition Reviews, 71(4), 221-231. https://doi.org/10.1111/nure.12015
Statista. (2023). Probiotic market size worldwide from 2019 to 2027. Retrieved from [Statista website URL if available].
Van Loo, J., Coussement, P., De Leenheer, L., Hoebregs, H., & Smits, G. (1995). On the presence of inulin and oligofructose as natural ingredients in the western diet. Critical Reviews in Food Science and Nutrition, 35(6), 525-552. https://doi.org/10.1080/10408399509527714
Ze, X., Duncan, S. H., Louis, P., & Flint, H. J. (2012). Ruminococcus bromii is a keystone species for the degradation of resistant starch in the human colon. ISME Journal, 6(8), 1535-1543. https://doi.org/10.1038/ismej.2012.4
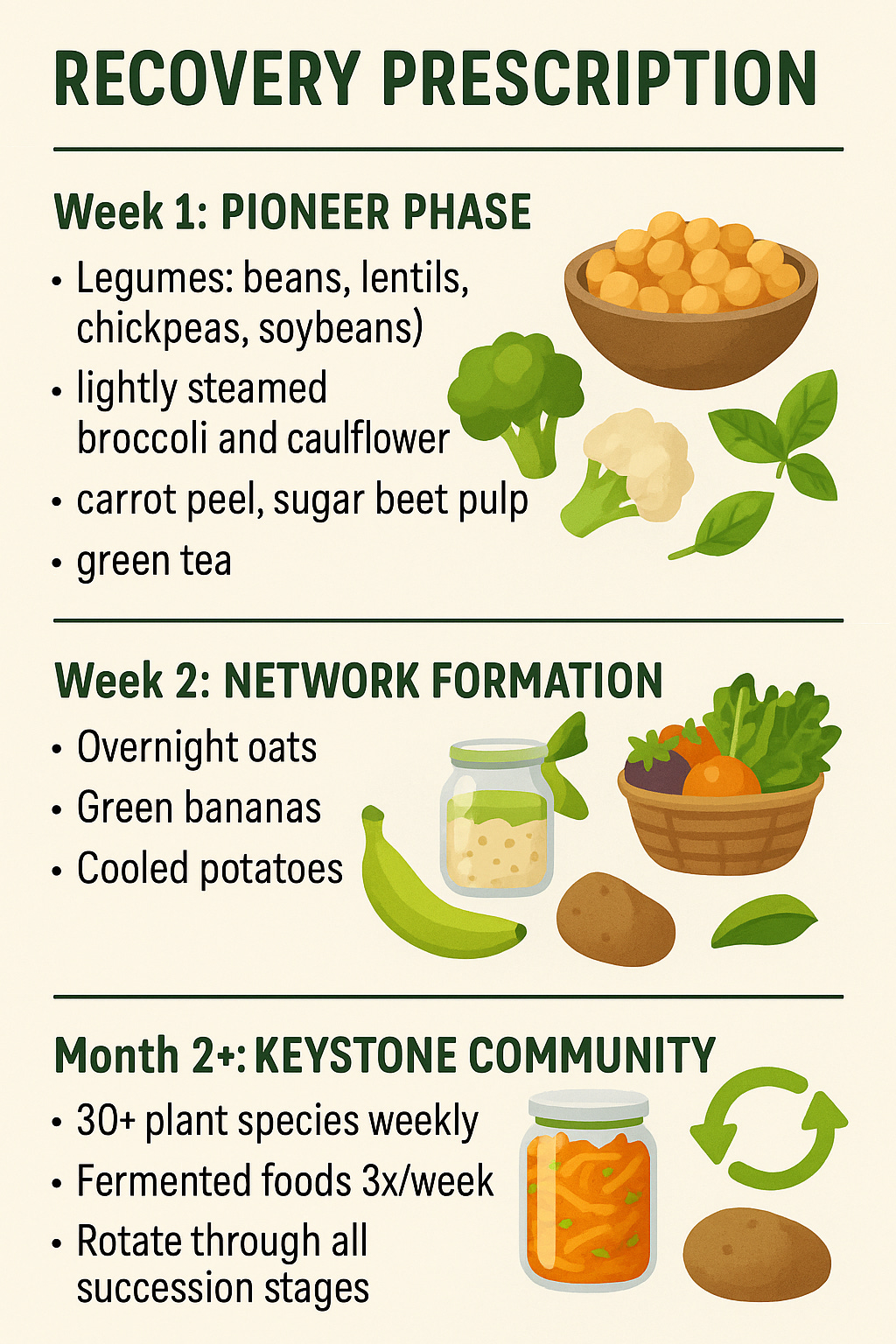
Recovery Prescription
Week 1: Pioneer Phase
· Legumes: beans, carrots, lentils, chickpeas, soybeans
· lightly steamed broccoli and cauliflower
· carrot peel, sugar beet pulp
· polyphenols: berries and green tea
Week 2: Network Formation
· Overnight oats
· Green bananas
· Cooled potatoes
· Onions
· garlic
Month 2+: Keystone Community
· 30+ plant species weekly
· Fermented foods 3x/week
· Rotate through all succession stages







Very nice and helpful article. One omitted consideration is that for some of us who have IBS or worse, high fiber foods are often a problem.